DynaMed® Medical Writer Amanda Thomason shares considerations for initiating insulin therapy in patients with type 1 diabetes. This is the second post in our series on insulin therapy for diabetes.
Types of Insulin
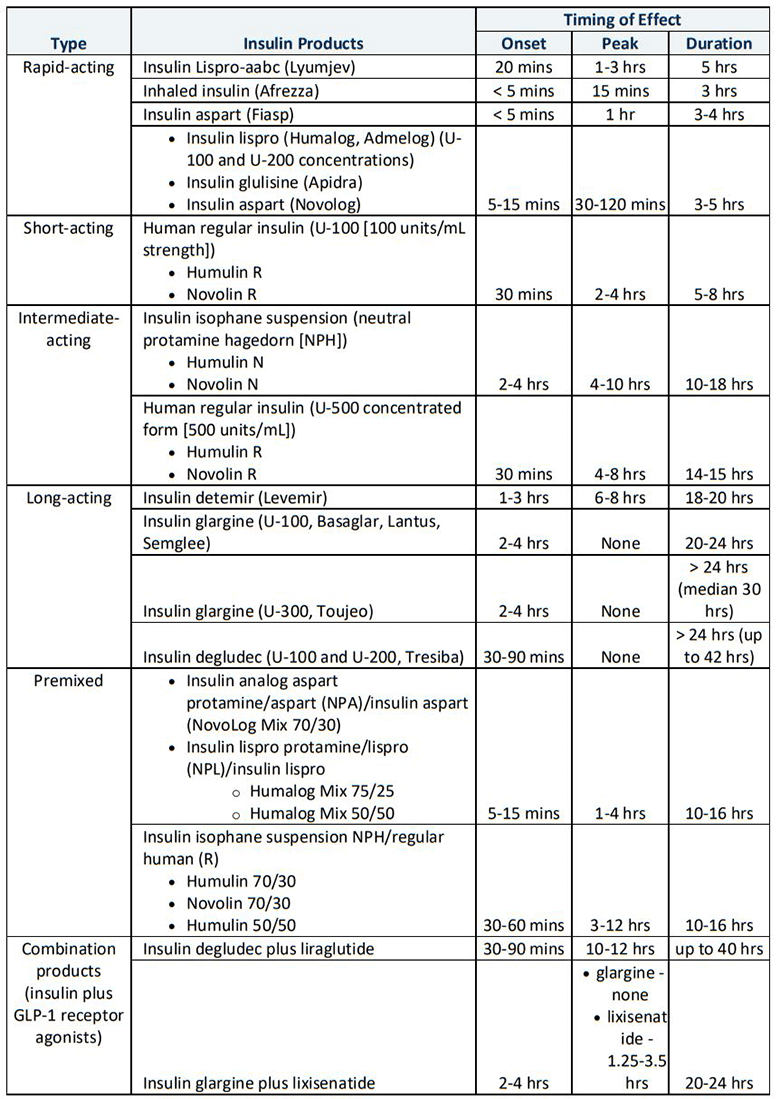
Insulin preparations range from rapid- to ultra-long-acting and include human and human analogs. The onset, peak and duration of action vary among types. The most common regular insulin and insulin analog concentration is 100 units/mL (U-100). However, more concentrated insulins exist (such as U-200 aspart and degludec, U-300 glargine, and U-500 regular), some of which have significantly different kinetics than the same medication at U-100 concentration. For example, U-300 glargine has lower hypoglycemia risk than U-100 glargine. The following table gives an overview of the various types of insulin available.
Insulin Regimens
Several insulin regimens are used in the treatment of type 1 diabetes:
- Basal insulin alone: typically, once daily injections of long-, ultra long-, or intermediate-acting insulin intended to correct fasting hyperglycemia and cover basal requirements
- Prandial (also known as bolus) insulin: bolus insulin injections to cover postprandial hyperglycemia (rarely given without some form of basal insulin)
- Basal-plus insulin therapy: basal insulin plus stepwise addition of one to three preprandial short-acting insulin injections per day, starting with a single bolus with the largest meal of the day
- Basal-bolus therapy: basal insulin plus boluses with meals/snacks intended to mimic physiologic insulin secretion (also called intensive insulin therapy or multiple daily injection therapy)
- Premixed insulin therapy: premixed, fixed dose formulations of long- or intermediate-acting insulins plus rapid- or short-acting insulins to approximate a basal-bolus regimen but with fewer injections
Insulin regimens for type 1 diabetes
Most patients with type 1 diabetes should be treated with basal-bolus therapy or with continuous subcutaneous insulin infusion (via insulin pump) plus boluses with meals/snacks. Rapid-acting insulin analogs for prandial insulin are recommended to reduce the risk of hypoglycemia. Premixed insulin therapy is also an option, though it is not as commonly used in patients with type 1 diabetes due to its lack of flexibility.
In general, insulin requirements can be estimated based on a patient’s weight with typical regimens consisting of doses ranging 0.4-1 units/kg/day (administered in divided doses with about half of total daily dose given as basal insulin and half as prandial). A patient’s carbohydrate intake, premeal blood glucose and expected physical activity should be considered when dosing prandial insulin. Note that higher amounts are required during puberty, pregnancy and acute illness.
Because sensitivity to insulin varies widely, dosing should be adjusted based on individual response to therapy. When adjusting insulin doses, depending on degree of hypo- or hyperglycemia and the patient's insulin sensitivity, it is reasonable to increase or decrease insulin dose by 10-20 percent and wait three to five days to assess the patient’s response.
A reasonable glycemic goal for many nonpregnant adults is a hemoglobin A1c (HbA1c) level lower than seven percent, but a patient’s goal should be based on individual factors. For example, in patients with a shorter duration of disease, longer life expectancy, or no significant cardiovascular disease, a more stringent target (such as HbA1c under 6.5 percent) may be reasonable if it can be achieved without significant hypoglycemia or other adverse effects. A less stringent target (such as HbA1c under eight percent) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, extensive comorbidities, or long-standing diabetes for whom goal is difficult to achieve.
Insulin therapy for patients with type 1 diabetes is a lifelong process. While the various options may seem daunting to the non-specialist, they provide flexibility for patients and, most importantly, some control over what their bodies cannot.
For more information, see DynaMed topics in the Insulin Management suite, including Initiating Insulin in Type 1 and Type 2 Diabetes and Insulin Infusion Devices.
Subscribe to our blog to be alerted of the next article in this series, which will explore types of insulin and regimens appropriate for people with type 2 diabetes, in addition to all the great articles from EBSCO Health Care.



